A physical trauma or a serious illness can render you temporarily “locked in”. Nevertheless, there are things that you want to know and things you want to communicate to others. Imagine waking up in an intensive care unit, hooked up to a ventilator and unable to move. You can make out that there are a number of people around you engaged in a range of activities and in conversations about you and about the interventions they are putting in place. How would you get their attention and once you got their attention, how would you communicate with them to find out where you are and what is going on? You want them to know that your mind is intact even if your body is not. You want them to treat you not just your body and most importantly you want to have some control over what kind of care you receive. The outcome of care is not just a function of the medical procedures and technical skills of our caregivers, but on our ability to be active participants in our care. Without effective patient-provider communication we cannot describe our symptoms and so run the risk of experiencing an adverse medical event that can lengthen our hospital stay or lead to a log term disability or even death.

We all want and believe that we can exercise the autonomy we had before the accident or disease limited our ability to speak and move, If we hadn’t planned ahead and had not prepared an advanced medical directive, how would we let folks know what we wanted. Or if we did have an advance medical directive on file, how would we let people know that we wanted them to follow it or that we wanted to make some changes.
Without an effective channel of communication, it is difficult for our caregivers to assess us and determine whether we are competent to participate in medical decision making and take an active role in our rehabilitation. The first and most rudimentary attempt at gauging our competence is to be able to somehow demonstrate that we can reliably respond to questions that only require a yes or no response. When you can’t speak, gauging your competence can be challenging. Good bedside practice should have caregivers try to identify a reliable way for their patient to indicate a yes and no response. Depending on how severely “locked in” you are, you could indicate yes and know with a thumbs up or down, one or two hand squeezes, or by looking up or down. To be effectively used everyone you interact with must be able to recognize which gesture you intended to produce. Sadly, producing two distinguishable gesture may be beyond what many ICU patients are capable of producing. But even if you can produce such yes/no gestures you still may have no effective way to summon your nurse if you are in pain or need something.
That is the depressing scenario that 30-50% of conscious mechanically ventilated patients face every day. They are trapped and unable to independently summon help or effectively communicate. To address the needs of these millions of patients, Voxello has taken the smart switch technology developed at the University of Iowa and produced the noddle switch that enables patients to summon help and control a speech generating device even if they can only produce a tiny intentional gesture like a tongue click or a small low force and displacement gesture of some body part. Using patented gesture detection and counting algorithms the noddle can do much more than the conventional switches that have been on the market. The gesture detection algorithm can reliably detect the intentional gesture like a tongue click and then count whether you produced one, two, or three gestures in a row. Base on the number of sequential gestures you produced, the noddle can either activate the nurse call system or allow you to navigate and select messages on the Voxello noddle-chat communication device.
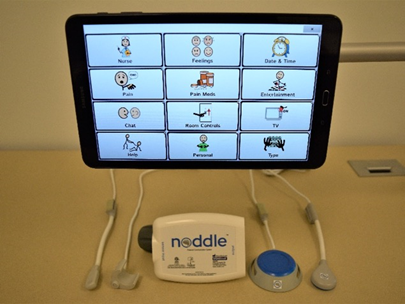
You don’t have to be one of those “locked-in” patients if you land up being hospitalized. Even if you can only produce a single intentional gesture, Voxello’s noddle smart switch and the noddle-chat communication tablet make it possible for you to be able to summon help and effectively communicate with their caregivers.
Have Questions? Contact us!
Richard Hurtig, Ph.D. Chief Scientific Officer
O: 319-333-7302 ext. 501 | C: 319-594-5404 | richardhurtig@voxello.com
